FAST & FREE 📦 3-DAY SHIPPING!*

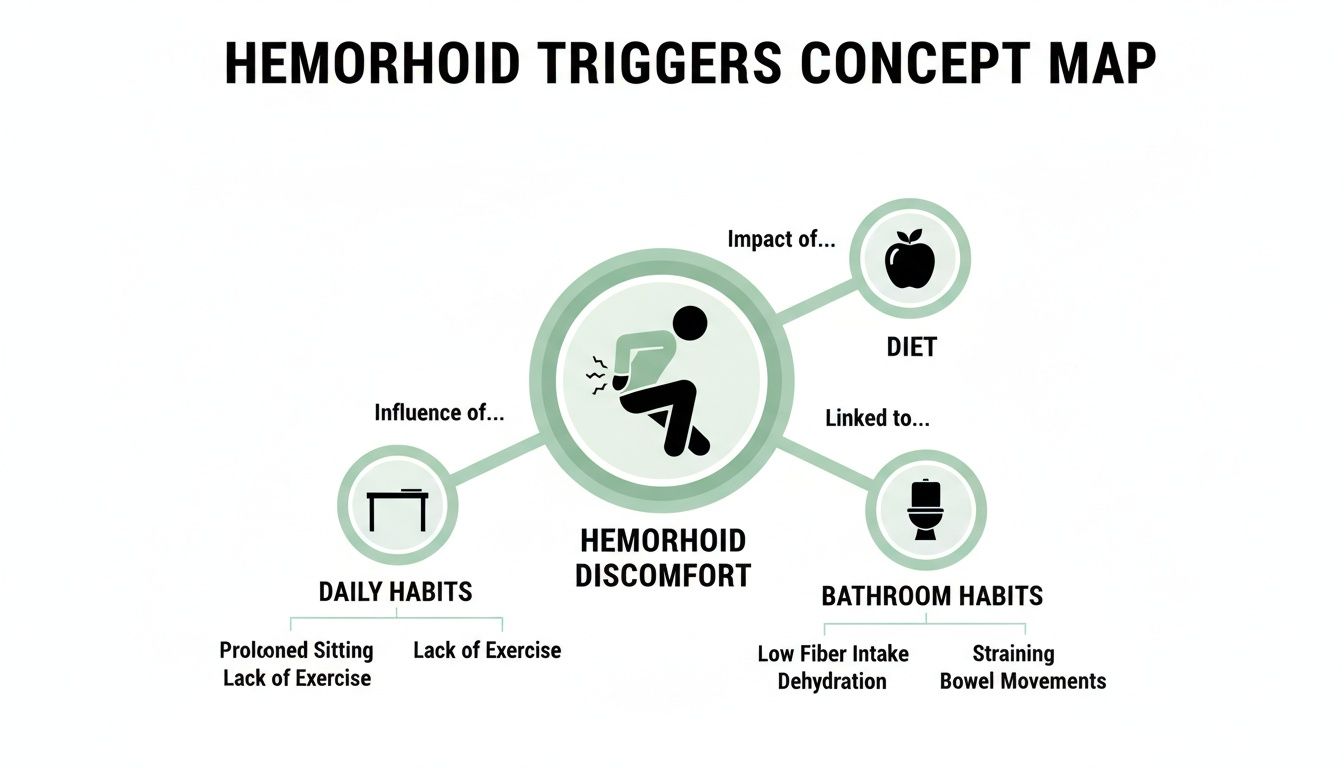
Most people don’t realize their daily routine is actually making their hemorrhoids worse. It's usually the small, innocent-looking habits… things like how you sit at your desk, what you grab for a quick lunch, or that extra ten minutes you spend scrolling on the toilet.
These things stack up, creating the perfect storm for pain and irritation.
It helps to think of hemorrhoids as tiny, delicate balloons. The root of the problem is anything that ramps up pressure in your lower abdomen, which forces blood into these veins and causes them to swell. Once you can spot these hidden pressure-triggers in your everyday life, you're on the path to lasting relief.
I once talked to a customer who was a long-haul truck driver, and he was completely baffled by his persistent hemorrhoids. He ate reasonably well and was pretty active when he wasn't on the road.
The problem wasn't one big thing... it was the combination of sitting for hours on end, the constant subtle vibrations from the truck, and his reliance on grab-and-go processed snacks during long shifts.
His story gets to the heart of the matter: hemorrhoids are rarely caused by a single event. They’re the result of accumulated pressure from many small, seemingly harmless daily habits.
Your daily routine will either starve your hemorrhoids or feed them... there is no middle ground.
This experience taught me that it's a battle won with consistency. It's not about finding a magic cream, though a quality product like Revivol-XR can provide essential, soothing relief. True, long-term comfort comes from dismantling the root causes of the pain, one small change at a time.
This guide will give you a clear roadmap to do just that. We’ll dive into:
By making a few small, informed adjustments, you can break the cycle of flare-ups and get your comfort back. It all starts with recognizing that your everyday choices have a direct and powerful impact on how you feel.
If there's one single dietary factor that consistently makes hemorrhoids worse, it’s a lack of fiber. Low-fiber diets are a direct pipeline to hard, dry stools that are a nightmare to pass, forcing you to strain on the toilet.
Think of your digestive tract like a water slide. A high-fiber diet with plenty of water keeps everything moving smoothly. But a low-fiber diet is like trying to go down that slide with no water... it creates friction, backup, and a whole lot of painful pressure right where you don't want it.

So many of our go-to convenience foods are notoriously low in fiber. They might be quick and easy, but they often contribute directly to constipation and those dreaded hemorrhoid flare-ups.
Processed foods are some of the biggest offenders. We're talking about white bread, pastries, most frozen dinners, and sugary cereals. The refining process strips away the fiber-rich outer layers of grains, leaving behind simple starches that can gum up your digestive works.
Other common culprits include:
You could be eating all the fiber in the world, but if you're not drinking enough water, it can actually make things worse. Dehydration is fiber's sneaky accomplice in aggravating hemorrhoids.
Fiber needs water to do its job. It soaks up water to soften and add bulk to your stool, making it much easier to pass. When you're dehydrated, your body pulls water out of your colon to use elsewhere, leaving behind hard, dry stools that are difficult to move.
Think of it this way: Fiber is the sponge, but water is what makes it soft. Without water, you’re just pushing a dry, abrasive sponge through your system.
Try to aim for at least 8 glasses of water a day. You'll need even more if you're active or it's hot outside. And no, coffee and alcohol don't count... in fact, they can dehydrate you even further.
The good news is you don’t have to completely change your diet overnight. Making small, consistent swaps can make a huge difference.
Here are a few actionable steps to take:
| Common Problem Food | How It Worsens Hemorrhoids | Smart High-Fiber Swap |
|---|---|---|
| White Bread & Pasta | Refined grains are stripped of fiber, slowing digestion and leading to hard stools. | 100% Whole-Wheat Bread, Brown Rice, Quinoa, or Whole-Grain Pasta |
| Sugary Cereals & Pastries | High in refined carbs and sugar with almost no fiber, contributing to constipation. | Oatmeal topped with berries and flax seeds, or a high-fiber bran cereal. |
| Cheese & Ice Cream | High in fat and low in fiber, dairy can be binding and slow down bowel movements for many people. | Greek Yogurt with fruit (probiotics help, too!), or a handful of nuts. |
| Red Meat (Beef, Pork) | Contains zero fiber and can be difficult to digest, leading to slower transit time in the colon. | Beans, Lentils, or Chickpeas in soups, salads, and chilis. |
| Chips & Fried Foods | High in unhealthy fats that slow digestion, and very low in fiber and water content. | An Apple with the skin on, a pear, a handful of almonds, or baby carrots. |
Dietary changes take time to work. For more immediate relief, a soothing product like Revivol-XR's Advanced Hemorrhoid & Fissure Cream can calm irritation and pain while you get your digestive health on track.
That truck driver I mentioned... his small daily habits were his biggest enemy. He had to learn that consistency with diet and hydration was the only way to get true, lasting relief on the road.
What happens behind the bathroom door can have a massive impact on a hemorrhoid flare-up. And the biggest offender is often a habit many of us share… sitting on the toilet too long, especially while scrolling on a phone or reading a book.
Think about how a toilet is designed. It leaves your rectum completely unsupported, letting gravity pull everything down. This posture causes blood to pool in the delicate veins of your lower rectum, ramping up the pressure and making hemorrhoids swell.

Straining during a bowel movement is another huge trigger. It’s more than just pushing hard... it’s the act of holding your breath and bearing down, a move doctors call the Valsalva maneuver. This action skyrockets the pressure inside your abdomen, forcing blood into the hemorrhoidal veins and causing them to bulge.
The problem doesn’t stop there. Using dry, abrasive toilet paper on already swollen and sensitive tissue is like rubbing sandpaper on a sunburn. Aggressive wiping can easily irritate the area, cause tiny tears, and lead to bleeding, dragging out the healing process.
Your bathroom should be for relief, not a place where you unknowingly make things worse. Spending more than five minutes on the toilet basically turns it into a pressure chamber for your hemorrhoids.
These habits feed into a vicious cycle. Straining worsens hemorrhoids, which can make you feel like your bowel movement is incomplete, leading you to sit longer and strain even more. Breaking that cycle is the key to finding real relief.
The good news is you can break these habits with a few simple adjustments. These small changes work by reducing pressure, protecting sensitive skin, and promoting faster healing.
Here are four things you can start doing today:
By simply being more mindful of what happens in the bathroom, you can eliminate some of the biggest factors that make hemorrhoids worse. For more tips, check out our guide on how to avoid straining during bowel movements.
For many women, pregnancy is an amazing journey, but it also brings a wave of physical changes that can create the perfect storm for hemorrhoids. The experience is incredibly common, often turning what should be a joyful time into one filled with nagging discomfort.
This isn’t just a small inconvenience; it's a major physiological challenge. Up to 40% of pregnant women in the U.S. will develop hemorrhoids, and the numbers often climb even higher in the postpartum period. This is no coincidence... it's the direct result of a body working overtime.

During pregnancy, three key factors team up, dramatically increasing the odds of a painful flare-up. Each one adds another layer of stress to the delicate veins in your rectal area.
First, your growing uterus puts immense, direct pressure on the veins in your lower abdomen and pelvis. Imagine these veins are a highway for blood returning to your heart. The uterus acts like a major roadblock, slowing down traffic and causing blood to pool.
Second, pregnancy hormones... especially progesterone... are busy relaxing your muscles to prepare for childbirth. But this relaxing effect also applies to the walls of your veins, making them much softer and more likely to swell under all that increased pressure.
Finally, constipation often becomes a constant companion during pregnancy. This can happen because hormones slow down digestion or because of iron supplements. The result is more straining on the toilet, which is one of the biggest single things that makes hemorrhoids worse.
Just when you think the pressure is off, childbirth arrives. The intense pushing and straining during labor can cause new hemorrhoids to form almost instantly or make existing ones severely inflamed.
For new mothers, this physical and emotional toll can feel overwhelming. A massive global meta-analysis involving 150 studies confirmed that pregnancy is a huge trigger, more than doubling a woman's risk for hemorrhoidal disease.
For new and expecting mothers, finding safe relief isn't a luxury... it's a necessity for physical and emotional well-being.
Unfortunately, the postpartum period doesn't always bring immediate relief. It takes time for your hormone levels to return to normal and for the pressure in your pelvic region to finally subside.
Because of the unique needs during this sensitive time, many OB/GYNs recommend steroid-free solutions. Products that focus on gentle, soothing ingredients can provide much-needed comfort without introducing harsh chemicals.
Here are a few gentle approaches that can help:
Managing hemorrhoids during and after pregnancy requires a gentle yet effective approach. For more detailed strategies, check out our guide on how to prevent hemorrhoids while pregnant.
Beyond diet and bathroom habits, certain parts of your daily routine can create the perfect storm for hemorrhoids. One of the biggest culprits is a sedentary lifestyle. If your job has you sitting at a desk or behind the wheel for hours on end, you're putting constant, direct pressure on the delicate veins in your rectum.
Think of it like standing on a garden hose. That prolonged pressure restricts blood from flowing out of the area, causing it to pool and swell. Over time, this chronic pressure is what can turn a minor annoyance into a recurring source of pain.
But it's not just sitting that causes problems. On the flip side, sudden bursts of intense physical strain can be just as damaging. Improperly lifting something heavy... whether you're at the gym or just moving furniture... creates a sharp spike in abdominal pressure.
This mimics the exact mechanics of straining on the toilet. When you hold your breath and bear down, you force blood into the rectal veins, which can trigger an immediate and painful flare-up. Being overweight also plays a big role, as the extra body weight adds to the chronic pressure on your entire pelvic region.
Think of your daily routine as a balance. Too much sitting creates constant, low-grade pressure. Improper lifting creates sudden, high-grade pressure. Both roads can lead to the same painful destination.
Recognizing these triggers is the first step. Making small adjustments can interrupt this cycle of pressure and pain, making a huge difference in your comfort.
The good news? You don’t need to quit your desk job or stop exercising to find relief. You can counteract these pressures with simple, practical changes you can start today.
Here are a few actionable steps to get you started:
These small tweaks can significantly dial down the daily stress on your rectal veins. You can learn more about how to choose the right activities in our guide, can exercise cause hemorrhoids.
Most of the time, you can manage hemorrhoids at home with lifestyle tweaks and the right products. But there are definitely times when self-care isn’t enough.
Ignoring certain warning signs can be risky, so it's important to know when to stop guessing and get a professional opinion. While hemorrhoids themselves aren't usually dangerous, they can mimic symptoms of more serious conditions. A proper diagnosis from a doctor gives you peace of mind.
Some symptoms are your body’s alarm bells, telling you it’s time to call a doctor right away. Don’t just wait and hope they disappear on their own.
Pay close attention if you experience any of these:
Getting a proper diagnosis is the most important step you can take. Your health is not something to gamble on.
Seeing a doctor isn’t about giving up… it's about being smart with your health. A professional diagnosis is key for a couple of big reasons.
First, it confirms you’re actually dealing with hemorrhoids and not something more serious like an anal fissure, an infection, or even colorectal cancer. Second, if your symptoms are severe, a doctor has access to more advanced treatments that aren't available over the counter.
Getting the right diagnosis opens the door to the right solution, helping you finally move past the pain and get back to your life.
When you’re dealing with a hemorrhoid flare-up, you’re bound to have questions. Getting clear, straightforward answers is the first step toward making smart choices for your health and feeling better faster.
Here are a few of the most common questions people ask about what makes hemorrhoids worse, with the practical information you need to get some relief.
Yes, they absolutely can, though the connection isn’t always direct. When you're stressed, your body pumps out hormones like cortisol that can throw your entire digestive system out of whack.
This often leads to constipation, which is one of the biggest culprits behind hemorrhoid flare-ups. On top of that, stress can make you unconsciously clench your pelvic floor muscles, ramping up pressure on the very veins that are already irritated.
For the most part, yes, but you have to be smart about it. Now is not the time for high-impact activities that increase pressure in your abdomen.
During a flare-up, it’s best to steer clear of:
Instead, switch to low-impact exercises that get your blood flowing without adding extra pressure. Think gentle walking, swimming, or specific yoga poses.
The goal of exercise during a flare-up is to gently support circulation, not to push through the pain.
The healing time really varies from person to person. For a mild case, you might start to feel relief from itching and minor pain within a week, as long as you’re consistent with home care... that means a high-fiber diet, lots of water, and no straining.
More severe or thrombosed hemorrhoids, however, can take two to three weeks or even longer to fully resolve. Consistency with your self-care routine is everything. If your symptoms don’t get better after a week, or if they’re severe, it's always a good idea to check in with your doctor.
At Revivol-XR, we know that managing hemorrhoids requires a comprehensive approach, from understanding triggers to finding effective, soothing relief. Our full line of products is designed to provide comfort at every step of your healing journey. For trusted, multi-symptom care, explore our solutions at https://hemorrhoid.com.