FAST & FREE 📦 3-DAY SHIPPING!*

Most people don’t realize that straining on the toilet for just five minutes can be the start of years of hemorrhoid pain. For many, the first sign of an internal hemorrhoid is a bit of a shock... and it often shows up without any pain at all. You might just see some bright red blood on the toilet paper or in the toilet bowl after a bowel movement. While it can be alarming, this is the most common calling card for internal hemorrhoids.

It usually starts quietly. I remember a client, a busy project manager, who came to us completely stressed. He’d noticed a bit of blood after using the restroom but felt zero pain, so he ignored it for weeks, thinking it would just go away.
He was so focused on his deadlines that he pushed his health to the side. But that silent signal is exactly what internal hemorrhoid symptoms often look like in the beginning. It wasn't until the symptoms got more disruptive that he finally sought help, realizing he wasn't alone in this.
Ignoring the quiet signs of a health problem only makes the problem louder later.
Believe it or not, my client was in the same boat as the 75% of Americans who will deal with hemorrhoid symptoms at some point. For internal ones, that signature symptom is painless, bright red bleeding. This issue accounts for about 4 million office and emergency room visits in the U.S. every year, making it a major-league concern that people often suffer through in silence until it becomes unbearable.
Figuring out these early signs is your first step toward getting relief. Unlike their external cousins, internal hemorrhoids are tucked away inside the rectum, so you usually can't see or feel them. This area also has fewer pain-sensing nerves, which is why discomfort isn't always part of the equation.
The symptoms can show up in different ways and sometimes change over time. Here are the main things to watch out for:
For a clearer picture, here is a quick summary of what to keep an eye on.
| Symptom | What It Looks or Feels Like | When It Typically Occurs |
|---|---|---|
| Painless Bleeding | Bright red blood on toilet paper or in the toilet bowl | Immediately after a bowel movement |
| Prolapse | A soft, fleshy lump protruding from the anus | During or after straining; may retract on its own |
| Mucus Discharge | A clear or yellowish fluid, causing moisture | Can occur with or without a bowel movement |
| Itching/Irritation | An annoying itch or raw feeling around the anus | Often caused by mucus discharge or a prolapsed hemorrhoid |
| Feeling of Fullness | A sensation of incomplete evacuation | After using the restroom |
This table helps break down the most common signals your body might be sending. It's important to remember that these symptoms can sometimes overlap with other conditions. You can get more context from our complete guide on general hemorrhoid symptoms.
The most critical thing to remember is that bright red blood is very different from dark, tarry stool. Bright red blood usually means the source is close to the rectum, like a hemorrhoid. Darker blood, on the other hand, suggests a problem much higher up in your digestive system and calls for immediate medical attention.
By recognizing these signs for what they are, you're already taking control of your health. That project manager I mentioned... he finally found relief once he understood what was happening and took simple, actionable steps. You can too.
Seeing blood after you've used the toilet is understandably alarming. But when it comes to internal hemorrhoids, it’s not only the most frequent sign but it’s also typically painless. That last part is key... it’s one of the big clues that helps tell hemorrhoids apart from other, more serious issues.
The blood you see will almost always be bright red. This is a good thing. It means the blood is fresh and hasn't traveled far, which points to a source very low down in the digestive tract... exactly where internal hemorrhoids live.
Think of internal hemorrhoids as swollen, delicate veins just inside your rectum. This area has a rich blood supply and is lined with sensitive tissue. When you have a bowel movement, the stool passes by these swollen veins. If the stool is hard or you’re straining, it can easily scrape against them.
That friction is all it takes to cause a bit of bleeding. The vessel walls are stretched thin and easily irritated, causing a small amount of blood to appear. It's really more of a surface scrape than a deep bleed, which is why you don’t feel pain and why it usually stops right after you're done.
People often ask how much blood is "normal" for a hemorrhoid. We're not talking about a lot. You'll likely just see a few streaks on the toilet paper, a couple of drops in the toilet bowl, or maybe a thin line on the stool itself. Heavy or continuous bleeding is not typical and is a sign you should call your doctor.
Understanding what internal hemorrhoid symptoms are really starts with getting familiar with this specific sign. While spotting blood is never fun, knowing the "why" behind it can take a lot of the anxiety out of the equation.
Most of the time, this kind of painless, bright red bleeding is something you can manage with simple changes at home. However, you should never try to diagnose rectal bleeding on your own. It's always best to get it checked out by a healthcare professional to be certain.
Here are the specific red flags that mean you should definitely make that call:
By paying attention to these details, you can learn to tell the difference between a common, manageable symptom and a potential warning sign. This empowers you to handle minor flare-ups confidently while knowing exactly when it's time to seek professional help.
Sometimes, an internal hemorrhoid can swell up so much that it starts to slip down from its usual spot high up in the rectum. When it pushes all the way through the anal opening, it’s called a prolapse. It's a key sign that an internal hemorrhoid has become more significant.
Think of it like a sock that’s been turned partially inside out... the inner lining has found its way to the outside.
A prolapsed hemorrhoid often feels like a soft, moist, grape-like lump right at the anal opening. It’s different from an external hemorrhoid, which is always on the outside. This prolapse can create a feeling of fullness, make it tricky to get clean, or just feel like something is there that shouldn't be.
Doctors have a pretty straightforward way of classifying prolapsed internal hemorrhoids. They use a four-grade system that describes how far they slip down and whether they go back inside on their own. Knowing these stages can help you explain your symptoms much more clearly to a doctor.
Bleeding is a common symptom at just about any stage, and this diagram shows where you might notice it.
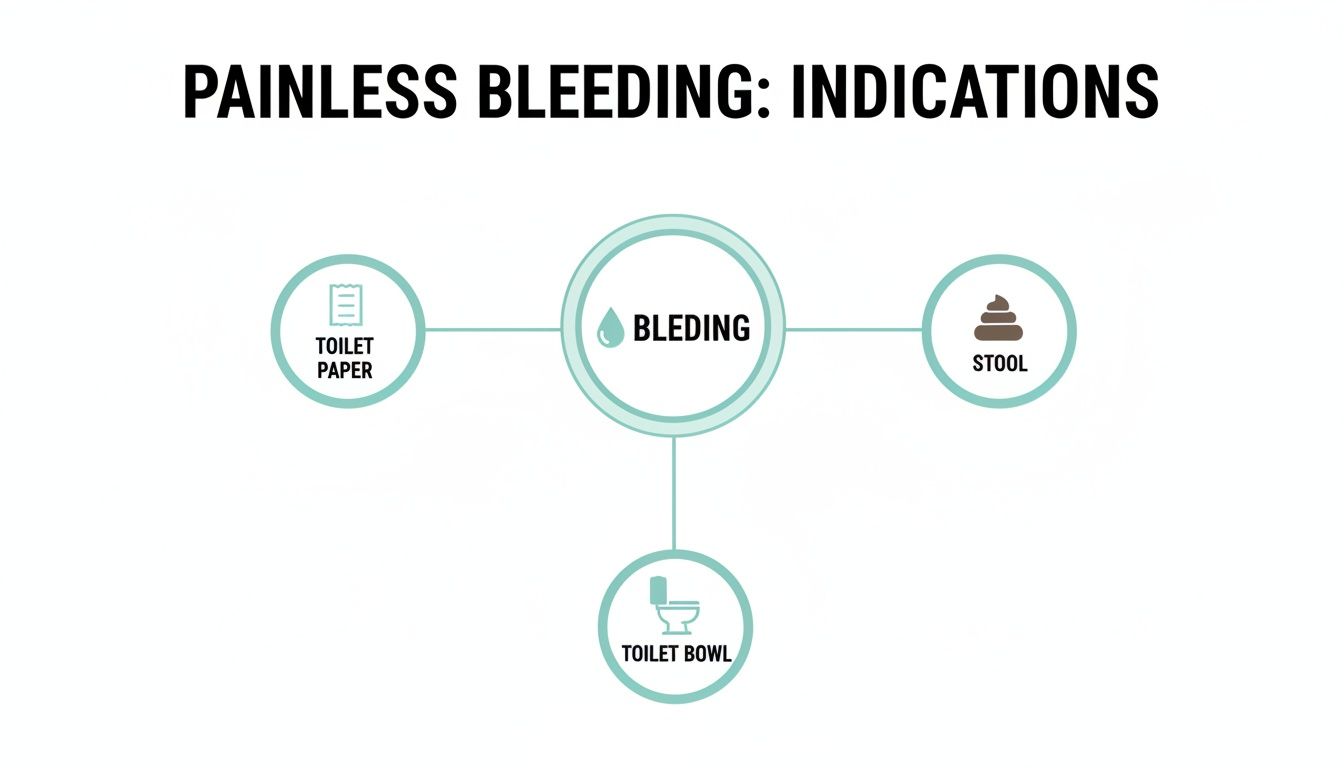
Whether you see a little blood on the toilet paper, drops in the bowl, or streaks on the stool itself, it’s a sign to pay attention to.
Here’s what’s important to remember... a prolapsed hemorrhoid can be alarming and uncomfortable, but it isn't always painful. The main issues are often just the physical presence of the lump, making hygiene a challenge, and the potential for irritation or mucus discharge.
If you have a hemorrhoid that has prolapsed, the key is to be gentle. Aggressive wiping will only make the irritation worse. Instead, try gently cleansing the area with water, a sitz bath, or a gentle toilet paper lotion after you go.
For a Grade 2 or 3 prolapse, you can often carefully push it back inside with a lubricated finger. This can really help reduce swelling and discomfort.
However, if a prolapsed hemorrhoid becomes very painful, turns a dark purple color, or feels hard, it might be "thrombosed." This means a blood clot has formed inside, and it needs immediate medical attention. Knowing these key differences will help you take the right steps for your own care.
Bleeding and prolapse might be the most well-known signs of internal hemorrhoids, but a few other symptoms can cause just as much daily frustration. These often fly under the radar, but they are a huge part of the full picture.
One of the most annoying is a mucus discharge. When an internal hemorrhoid slips down, it can drag the mucus-producing lining of the rectum along with it. This can leave you with a constant feeling of dampness and leakage that’s not only uncomfortable but also makes staying clean a real challenge.
That persistent moisture leads directly to another maddening symptom… itching. The medical term is pruritus ani, but all you need to know is that the mucus irritates the incredibly sensitive skin around your anus. This creates an intense urge to scratch or wipe, which only makes the irritation worse. It’s a vicious cycle. You can learn more about why hemorrhoids can be so itchy in our detailed guide.
This cluster of symptoms often shows up together:
These issues can really disrupt daily life. This is especially true for groups like pregnant or postpartum women, where up to 40% may deal with hemorrhoids from increased pressure. It's a global problem, and studies show that while many cases don't have symptoms, the irritation from mucus is a frequent complaint for those who do. You can read more about the full scope of these symptoms and their impact here.
Another incredibly frustrating symptom is the feeling that you haven't completely finished a bowel movement. A swollen or prolapsed internal hemorrhoid can create a sense of fullness or pressure inside the rectum, tricking your brain into thinking there’s still more to pass.
This sensation often leads people to strain on the toilet, which is just about the worst thing you can do for hemorrhoids. Straining increases the pressure on those already swollen veins, making the prolapse, bleeding, and discharge even worse.
Key Takeaway... Mucus, itching, and a feeling of fullness aren't just minor annoyances. They are real symptoms that can seriously impact your quality of life. Recognizing them as part of the internal hemorrhoid experience is the first step toward finding relief.
Knowing the signs of internal hemorrhoids is one thing, but getting an official diagnosis from a doctor is what really matters. It’s easy to feel a bit embarrassed, but trust me, your doctor has seen this countless times. The whole process is usually quick, surprisingly straightforward, and gives you the clarity you need.
Most appointments kick off with a simple chat about your symptoms and medical history, which then leads into a physical examination.
First, your doctor will likely perform a quick visual check of the anal area. They’re looking for obvious signs of external hemorrhoids, skin tags, fissures, or internal hemorrhoids that have prolapsed (slipped out).
Next up is usually a digital rectal exam (DRE). For this, the doctor puts on a glove, uses some lubricant, and gently inserts a finger just a short way into your rectum. It might sound a little awkward, but it’s over in seconds. This simple step allows them to feel for any abnormal growths or swollen tissue, including internal hemorrhoids.
If the hands-on exam doesn’t tell the whole story, your doctor might need a better look. That's where a procedure called an anoscopy comes in. It’s the best way for a doctor to get a direct view of the tissue inside your rectum.
This is the most common and reliable way to officially diagnose internal hemorrhoids.
A proper diagnosis is non-negotiable because it rules out other, more serious conditions that can also cause rectal bleeding. Getting checked ensures you're treating the right problem from the start.
While most hemorrhoid symptoms are more annoying than dangerous, some signs should absolutely not be ignored. Think of these as "red flags" that warrant an immediate call to your doctor, as they could point to a completely different issue.
Paying attention to these warnings is a crucial part of taking control of your health. When in doubt, always get it checked out.

Thankfully, you can often manage internal hemorrhoid symptoms right at home with a few simple, powerful adjustments. The idea is to reduce strain, soothe the irritation, and give your body a real chance to heal.
Here are concrete steps you can take today:
While at-home care is often very effective, you need to know when to call in a professional. It's time to stop self-treating and consult your doctor if:
These are red flags that you might need a different approach. Your doctor can give you an accurate diagnosis and make sure you get the most effective care for your specific situation.
When you’re dealing with something as personal as internal hemorrhoids, you’re bound to have questions. Getting straightforward answers is the first step toward feeling more in control and finding relief. Let’s tackle some of the most common questions we hear.
Most of the time, no. The strange thing about internal hemorrhoids is where they’re located... in a part of the rectum with very few nerves that register sharp pain. That’s why the classic sign of an internal hemorrhoid is painless bleeding, not agony.
So, when does pain become a factor? It usually happens if an internal hemorrhoid prolapses (slips out of the anus) and gets trapped by the surrounding muscles. This can cut off its blood supply, leading to a "strangulated" hemorrhoid, which is a painful and urgent medical issue. But for most people, the sensation is more like pressure or fullness rather than actual pain.
They often can, especially if you catch them early. For minor cases, simple at-home adjustments can make all the difference. Focusing on adding fiber to your diet and drinking more water helps soften your stool, which is a game-changer.
When you don't have to strain, you give those swollen veins a chance to heal and shrink back to normal. If symptoms are a bit more stubborn or a hemorrhoid has prolapsed, over-the-counter treatments can help speed things along. The real key, though, is being consistent with your self-care routine.
The biggest difference comes down to one thing... location. And that location changes everything about how they feel. Internal hemorrhoids form inside the rectum, while external ones pop up under the skin right around the anal opening.
Think of it this way... the skin on the outside of your body is loaded with sensitive nerve endings. Because external hemorrhoids are right there, they're the ones that tend to be itchy, sensitive, and downright painful. Internal hemorrhoids, tucked away inside, are mostly known for that painless bleeding and a feeling of fullness.
For a complete approach to managing your symptoms and finding lasting comfort, explore the full range of solutions from Revivol-XR. Our doctor-trusted products are designed for targeted relief, helping you get back to your life without disruption. Visit https://hemorrhoid.com to find the right care for you.
Comments will be approved before showing up.