FAST & FREE 📦 3-DAY SHIPPING!*

Most people don’t realize their daily routine is actually making their hemorrhoids worse.
It’s a frustrating cycle. I remember a client who stopped going to the gym entirely out of fear. He thought any activity would aggravate his hemorrhoids, so he became sedentary. Over the next few months, he found that sitting all day made the pressure, pain, and constipation far worse than his workouts ever did. He felt trapped, believing he had to choose between being active and being in pain.
His story is incredibly common. People are told exercise is good for them, but the thought of any movement that might cause a flare-up is terrifying. So, they stop moving, and the problem escalates. It’s a classic case of the perceived solution becoming part of the problem.
The right kind of movement is your best tool for relief and prevention... not the enemy.
The answer to "does exercise help piles?" is a definite yes, but with a critical caveat. It has to be gentle, supportive movement. Strenuous, high-impact activities can increase abdominal pressure and worsen swelling. Consistent, low-impact activity, on the other hand, boosts blood flow, promotes healthy digestion, and strengthens the muscles that support your rectal area. This is the foundation for lasting relief.
This guide is here to give you confidence and clarity. I'll show you how to make exercise a cornerstone of your plan to manage hemorrhoids, not make them worse. Your path to feeling better starts with understanding how to move your body correctly.
To get started, it helps to know which activities help and which ones hurt. This quick-reference guide breaks it down for you.
| Activity Type | Risk Level | Why It Matters |
|---|---|---|
| Walking and Swimming | Safe (Green Light) | Low-impact, boosts blood flow, and reduces pressure. |
| Pelvic Floor Exercises | Safe (Green Light) | Strengthens supportive muscles without straining the area. |
| Prolonged Cycling | Avoid (Red Light) | Puts direct, sustained pressure on the sensitive perineal area. |
| Heavy Weightlifting | Avoid (Red Light) | Dramatically increases internal pressure, worsening symptoms. |
Understanding this distinction is the first step. By choosing your activities wisely, you can use movement to improve circulation, ensure regularity, and ultimately reduce the strain that leads to flare-ups.
To see how exercise helps, think of your circulatory system as a web of tiny rivers. When you’re still for a long time, blood flow slows down, like water in a stagnant pond.
This lets pressure build up in delicate veins... including the ones around your anus.
This is exactly why sitting for hours often makes hemorrhoid pain worse. The right kind of movement gets things flowing again, offering relief in three important ways.
Gentle physical activity acts like a natural pump for your blood vessels. A brisk walk or a few easy laps in the pool gets your heart rate up just enough to improve circulation throughout your body.
This healthier blood flow helps move the pooled blood out of the swollen veins in your rectal area. As that trapped blood starts moving freely again, the painful pressure and swelling that define a hemorrhoid flare-up begin to go down.
This diagram shows how these benefits connect.
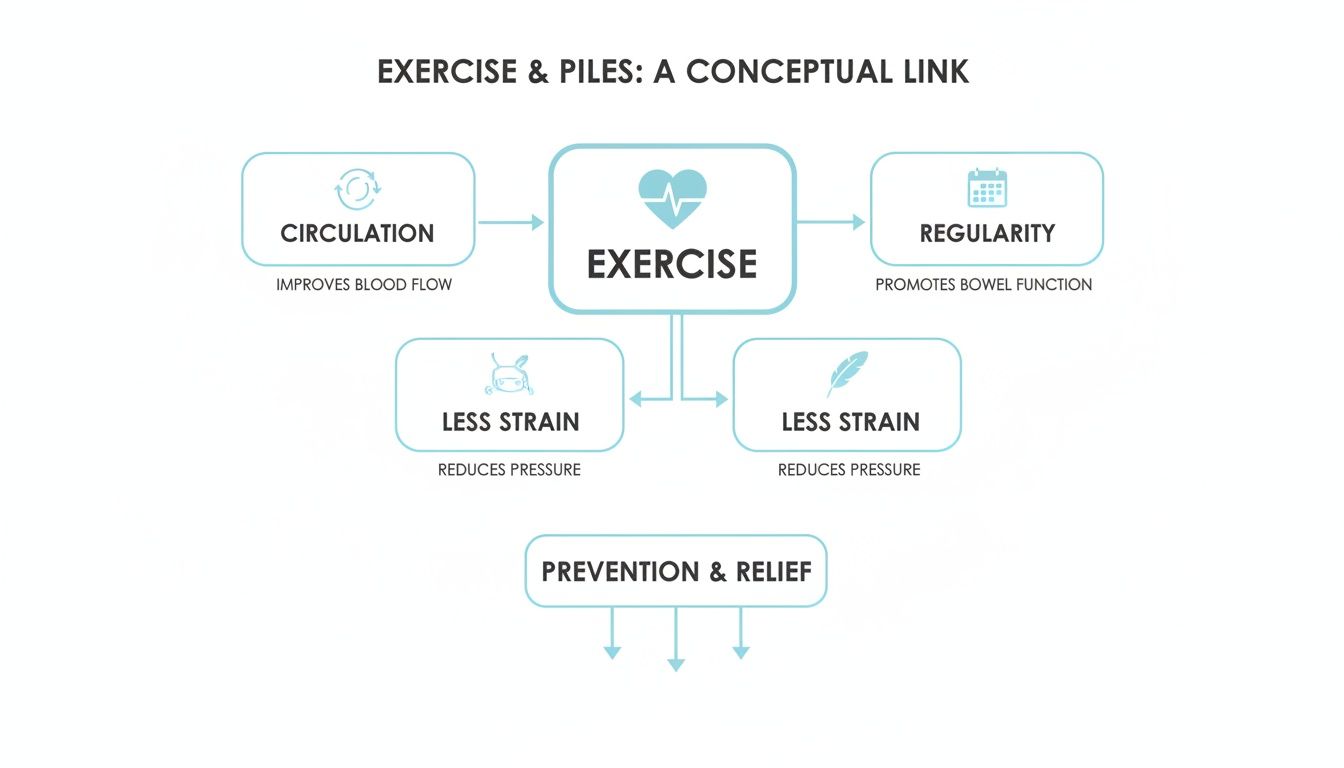
As you can see, exercise improves circulation, promotes regular bowel function, and reduces strain... all key factors in managing piles.
Constipation is one of the biggest triggers for hemorrhoids. When you have to strain to pass a bowel movement, you put tremendous pressure on the rectal veins, causing them to swell up and become painful.
Exercise is a fantastic, natural way to keep your digestive system on track. Physical activity stimulates the muscles in your intestines, which helps move waste through your system more efficiently.
When your bowel movements are regular and soft, you don't need to strain. This simple change is one of the most powerful things you can do to prevent new hemorrhoids and give existing ones a chance to heal.
Your core and pelvic floor muscles are like a support system for your lower abdomen's organs and veins. If these muscles are weak, more pressure is put on the sensitive veins in the rectal area.
Specific exercises, which we’ll cover in a bit, help strengthen this internal "girdle."
This provides better support and stability, easing the constant downward pressure that contributes to hemorrhoids. It's like building a stronger foundation to keep the walls from cracking.
The connection between regular activity and hemorrhoid relief is well-established. Clinical reviews recommend 20–60 minutes of moderate physical activity, 3–5 days per week, to improve bowel function and manage symptoms. In fact, studies show that combining lifestyle changes like exercise with more dietary fiber leads to a major drop in persistent symptoms and roughly a 50% decrease in the risk of bleeding. This data underscores how consistent, gentle movement is a cornerstone of effective hemorrhoid management. You can read the full research about these lifestyle findings here.
Now that we know how movement helps, let's get practical. Think of this as your playbook for safe, effective exercises that can actually help you heal and feel better.
The whole game is about choosing low-impact activities that get your blood flowing without adding pressure where you don't want it.

When it comes to hemorrhoid-friendly exercise, walking is the undisputed champion. It’s simple, free, and offers the perfect balance of benefits. A brisk 20 to 30-minute walk each day is all it takes to get your digestive system moving and give your circulation a meaningful boost.
This gentle rhythm encourages blood to flow away from the swollen rectal veins, which helps dial down pain and inflammation. It's also a powerful weapon against constipation. For a deeper look, check out our guide on is walking good for hemorrhoids.
For a truly zero-impact workout, the pool is your best friend. Swimming and water aerobics are fantastic because the water’s buoyancy supports your entire body, taking nearly all the pressure off your pelvic floor and lower back.
This weightless environment lets you get a great cardio workout without any jarring movements. As a bonus, the cool water can be incredibly soothing for external hemorrhoids.
Strengthening your body's internal support system is a game-changer for long-term hemorrhoid management. Pelvic floor exercises, often known as Kegels, tone the very muscles that support your rectum. A stronger pelvic floor means less strain on the veins in that area.
Here's how to do them right:
The best part? You can do them anywhere... at your desk, in the car, or while watching TV.
Small pilot studies have shown that targeted exercise can lead to significant symptom reduction. A six-week Pilates program, for example, resulted in major improvements in constipation and internal hemorrhoid severity. Similarly, a study combining conservative care with Kegel exercises found highly significant improvements in hemorrhoid symptoms within just one month. You can learn more about these promising exercise findings here.
Certain yoga poses can be amazing for improving blood flow and releasing the deep-seated tension that makes hemorrhoid pain worse. The key is to stick with gentle stretches that don’t put pressure on your abdomen.
You’ll want to avoid poses that involve intense core work or holding your breath, as this can ramp up internal pressure. Instead, focus on movements that feel restorative.
Safe Poses to Try:
While the right kind of movement can bring a lot of relief, it's just as important to know which activities can make hemorrhoids worse.
Not all exercise is created equal. Some popular workouts can spike internal pressure, leading to more pain and swelling.
The goal isn't to make you give up the activities you love. It’s about being smart and making a few tweaks to protect yourself from a flare-up.

Lifting heavy weights... especially squats, deadlifts, or leg presses... is one of the riskiest things you can do with active hemorrhoids. The problem isn’t just the heavy load; it's how we instinctively breathe when we lift.
Many people perform the Valsalva maneuver without even realizing it. This is when you hold your breath and bear down during the toughest part of a lift. This action creates a huge spike in intra-abdominal pressure. Think of it like squeezing a balloon... that pressure has to go somewhere, and it often goes right to the delicate veins in your rectum, causing them to bulge.
How to Modify Your Lifting Routine:
Some activities put direct, constant pressure on the perineal area. This can aggravate existing piles or even help new ones form by interfering with blood flow and causing irritation.
This isn’t just a theory. A study of over 300 athletes found that while 34% of participants reported having hemorrhoids, the numbers were far higher in certain sports. The prevalence shot up to a staggering 57% for cyclists and horseback riders and 48% for bodybuilders. This data clearly shows a link between activities that involve heavy straining and long periods of sitting. You can discover more insights about these activity-specific risks here.
This also underscores why understanding the connection between sitting too long and hemorrhoids is so important for managing your symptoms.
Exercises to Modify or Approach with Caution:
Exercise is a powerful tool, but it works best when it’s part of a complete strategy for relief. Think of it as one strong pillar supporting your recovery... it’s much more effective when combined with other smart habits.
Here is how you can take action.
A holistic plan addresses hemorrhoids from every angle, from what you eat to how you soothe immediate pain. This complete approach ensures you're not just managing symptoms but also preventing future flare-ups, making it possible to stick with your exercise plan long-term.
You can’t out-exercise a bad diet, especially when it comes to hemorrhoids. Constipation is a primary trigger, and the best way to fight it is from the inside out. Your goal is to make bowel movements soft and easy to pass, which eliminates straining.
By making these simple adjustments, you create the ideal internal environment for healing. You can learn more about specific ingredients by checking out our guide on foods that are good for hemorrhoids.
What you do in the bathroom matters just as much as what you do in the kitchen or the gym. Many people unknowingly make their hemorrhoids worse through poor toilet habits.
The biggest mistake is straining or pushing too hard. Another common problem is spending too much time on the toilet. Sitting for extended periods... often while scrolling on a phone... allows blood to pool in the rectal veins, increasing pressure and swelling.
The rule of thumb is if a bowel movement doesn't happen within a few minutes, get up and try again later.
While exercise and diet work on prevention, sometimes you need immediate relief from pain, itching, and swelling. This is where soothing therapies come in.
A warm sitz bath is one of the most effective at-home treatments. Soaking the affected area in warm water for 15 to 20 minutes several times a day can work wonders. It helps relax the anal sphincter, improve blood flow, and reduce inflammation.
For targeted, fast-acting relief, a high-quality topical treatment is an essential part of your plan. This is especially true when pain or itching makes it hard to even think about being active.
A product like Revivol-XR Advanced Hemorrhoid & Fissure Cream is designed for this very purpose. It combines a powerful numbing agent to block pain with ingredients that help shrink swollen tissue. This allows you to manage the acute symptoms that might otherwise stop you from getting the gentle exercise your body needs to heal.
That client I mentioned earlier, the one who quit the gym? He finally found relief when he stopped seeing exercise as the enemy and started seeing it as a partner in his healing. He swapped heavy lifting for brisk walking and swimming. He focused on hydration and fiber. This combination of gentle movement and smart lifestyle changes was the key that finally broke the cycle of pain.
Smart self-care isn’t just about home remedies... it’s also about knowing when to call in a professional. While the right exercises and lifestyle tweaks are great for managing hemorrhoids you know you have, they can't replace an official diagnosis from a doctor.
Only a clinician can confirm your symptoms are actually from hemorrhoids and rule out other, more serious issues.
Certain symptoms are more than just a nuisance; they're signals that you need a medical opinion. You should see a doctor as soon as possible for any of the following:
Your journey to relief starts with getting clear on what's going on. A doctor can perform a quick, simple exam to confirm the diagnosis and figure out the grade or severity of your hemorrhoids.
From there, they can recommend the best approach, whether that’s prescription medication, specific lifestyle changes, or in some cases, a minor procedure. Knowing exactly what you’re dealing with lets you take control of your health with confidence.
Remember, the information here is for educational purposes. Always talk to a healthcare provider about any medical concerns or before starting a new treatment.
Trying to figure out how to exercise with piles can bring up a lot of questions. Here are some straightforward answers to the most common concerns.
A thrombosed hemorrhoid... a blood clot inside an external hemorrhoid... is intensely painful. During this acute phase, your top priorities are rest and healing.
We strongly advise against any real exercise until the severe pain and swelling have gone down. Once you're feeling better, you can carefully reintroduce movement with very slow, short walks. Most importantly, always check in with your doctor for guidance.
Patience is everything after a medical procedure. You must follow your surgeon's specific post-op instructions, as they know the details of your case.
Typically, your first approved activity will be short, gentle walks to get your circulation going. You will need to strictly avoid any straining, heavy lifting, or intense core work for several weeks. Doing too much too soon risks damaging the surgical site.
This is a tricky one, and the answer really depends on the person. For some people, the high-impact jarring motion of running can be very aggravating to swollen, sensitive tissues.
If you want to try running, we suggest a cautious approach:
Yes, traditional sit-ups and crunches are best avoided if you have piles. These classic ab exercises create a significant spike in intra-abdominal pressure. This is the exact same type of internal strain that happens when you lift something heavy.
This pressure bears down directly on the pelvic floor and rectal veins, which can easily cause hemorrhoids to swell up and become more painful. Safer alternatives like planks, bird-dog poses, and glute bridges strengthen your core muscles effectively without creating dangerous downward pressure.
When flare-ups happen, managing symptoms is key to staying on track with your gentle exercise plan. Hemorrhoid.com offers the Revivol-XR Advanced Hemorrhoid & Fissure Cream, combining a powerful numbing agent with ingredients to reduce swelling, giving you the comfort you need to keep moving toward recovery. Learn more at https://hemorrhoid.com.
Comments will be approved before showing up.