FAST & FREE 📦 3-DAY SHIPPING!*

Most people don’t realize their daily routine is actually making their hemorrhoids worse.
I once watched a customer break down in tears because they thought their hemorrhoids would never go away. They’d tried everything... or so they thought. They were stuck in a cycle of temporary fixes, missing the one thing that could offer real, lasting relief. It was a heartbreaking moment, but it taught me a powerful lesson about the search for the best internal hemorrhoid treatment. People don’t just want a cream... they want a solution.
The best internal hemorrhoid treatment addresses both immediate symptoms and the underlying cause.
This means you need a two-part strategy. First, you need something that gives you quick relief from the itching, burning, and bleeding. This is where at-home care shines. But for a long-term fix, especially for stubborn flare-ups, you often need a professional approach that targets the problem at its source. Understanding when to use each approach is the key to finally getting off the hemorrhoid roller coaster.
To take action, you should:
That customer’s story wasn’t just about their pain... it was about the frustration of not knowing what to do next. Finding the best internal hemorrhoid treatment is about having a clear plan... knowing when to self-treat and when to seek professional help for a more permanent solution.
Internal hemorrhoids can cause a surprising amount of discomfort, from itching to bleeding. Thankfully, there are plenty of ways to treat them. The trick is to match the approach to the severity of your flare-up. Your options generally fall into two buckets: at-home care and professional medical procedures.
Most people start with at-home treatments. They’re easy to get, affordable, and work well for mild to moderate symptoms. This includes everything from simple lifestyle shifts to over-the-counter (OTC) products made to soothe irritation and shrink swollen tissue.
When you're dealing with the misery of internal hemorrhoids, seeing your options laid out clearly helps. The best choice is often a balance between getting relief now and finding a solution that lasts.
Here’s a quick comparison of the main approaches:
| Treatment Type | Primary Goal | Best For | Invasiveness |
|---|---|---|---|
| At-Home Care | Symptom management and immediate relief | Mild to moderate flare-ups | Non-invasive |
| Medical Procedures | Long-term resolution and prevention | Persistent or severe cases | Minimally invasive |
At-home care is all about calming the flare-up you’re dealing with today. This usually involves:
On the other hand, medical procedures are for when at-home methods just aren't cutting it. A doctor performs these treatments to provide a more permanent fix, usually by removing the hemorrhoid or cutting off its blood supply so it shrinks and falls off.
The best treatment plan usually starts with consistent at-home care. If your symptoms are still hanging around after a week... or getting worse... that’s a good sign it's time to talk to your doctor about more advanced options for lasting relief.
Choosing the right internal hemorrhoid treatment really boils down to one question: Are you looking for fast relief from a minor flare-up, or a more permanent fix for a problem that keeps coming back? It can feel overwhelming, but understanding the key differences between at-home care and in-office procedures makes the decision much clearer.
Think of at-home care as your first line of defense. It's affordable, easy to access, and works well for managing the symptoms of mild to moderate internal hemorrhoids. The goal here is to soothe irritation, calm down the swelling, and make smart lifestyle changes to keep them from coming back.
Medical procedures, on the other hand, are for more stubborn or severe cases. They do require a doctor's visit and are more hands-on, but they offer a long-term solution by getting rid of the problem tissue for good.
One of the biggest things to consider is whether you need relief now versus how long you want that relief to stick around. At-home treatments, like an over-the-counter suppository with phenylephrine, can start shrinking swollen tissue in just a few hours. That's great for getting quick comfort from itching and discomfort. But it's temporary... you have to keep using it.
In-office procedures work on a different timeline. A treatment like rubber band ligation provides a permanent fix, but the results aren't instant. The hemorrhoid usually shrinks and falls off within a week or two, but that comes after scheduling an appointment and allowing for a little recovery.
At-home care gives you speed and convenience for immediate symptom control... Medical procedures trade a bit of that speed for a more permanent, lasting solution.
This visual guide can help you map out your next steps based on what you're experiencing.
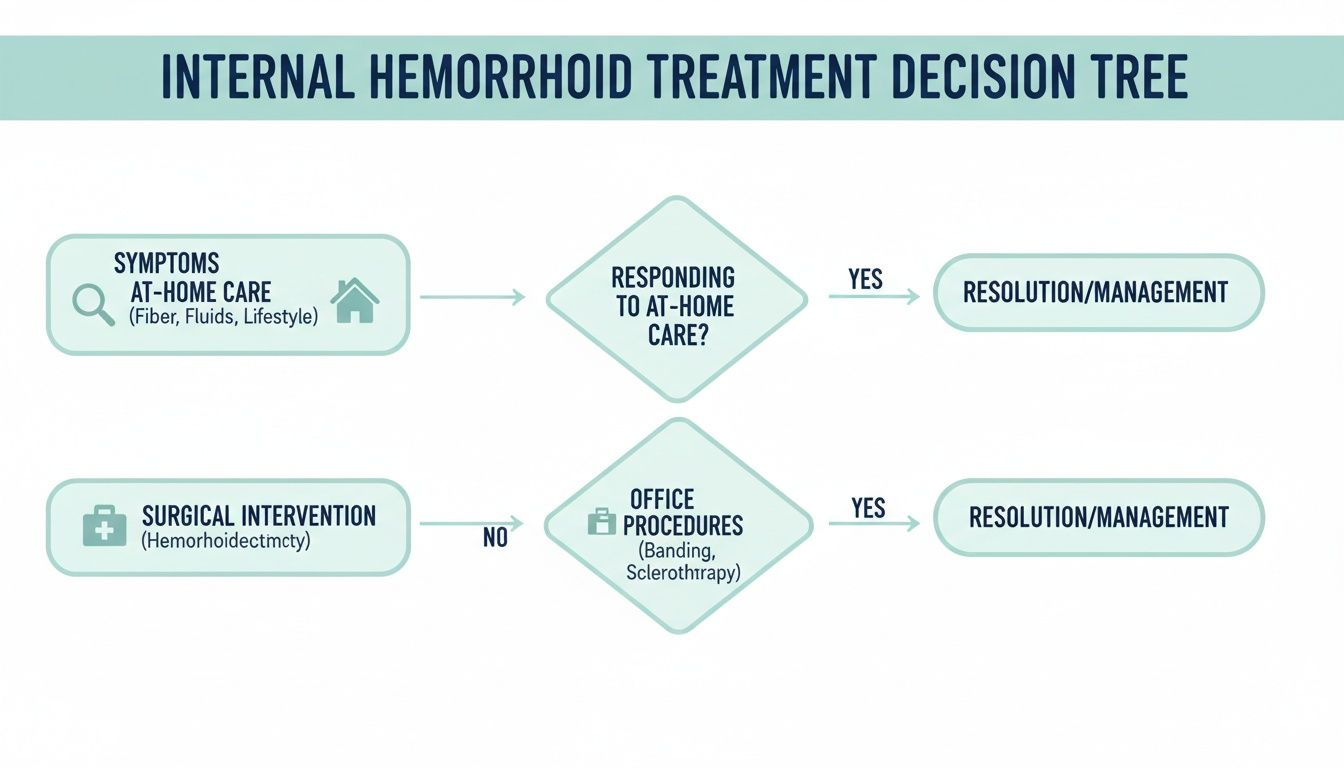
As the chart shows, the path to relief starts by figuring out your symptoms. That will point you toward either self-care at home or a conversation with your doctor about a medical procedure.
Let's talk about the practical side of things. At-home remedies are much easier on your wallet. A box of suppositories, some sitz bath salts, and adding more fiber to your diet are all low-cost ways to find comfort. Plus, they're completely non-invasive, so you can use them safely and privately at home. You can learn more about how these work by reading our guide on what a hemorrhoid suppository does.
Medical procedures have a higher upfront cost, though your insurance might cover a good portion of it. And while treatments like rubber band ligation are considered minimally invasive... they're done right in the doctor's office... they're still a bigger step than using a cream or suppository.
To make things simple, here's a look at how these two approaches stack up.
This table breaks down the key differences to help you decide which path makes the most sense for your situation right now.
| Treatment | Best For | Speed of Relief | Cost | Long-Term Solution | Key Benefit |
|---|---|---|---|---|---|
| At-Home Care | Mild to moderate flare-ups (Grade I-II) | Fast (hours to a day) | Low ($) | No (symptom management) | Immediate comfort & convenience |
| In-Office Procedures | Persistent or severe cases (Grade II-III) | Gradual (1-2 weeks for full results) | Moderate-High ($$$) | Yes (permanent fix) | Solves the root problem |
Ultimately, the best choice depends on how much your symptoms are impacting your daily life and whether you're looking for a quick patch or a lasting solution.
When you look at the long game, medical procedures clearly have the upper hand. For those dealing with internal grade II and III hemorrhoids, rubber band ligation (RBL) is a true standout. It's simple, recovery is fast, and it often delivers the best 1-year results among nonsurgical options. With success rates estimated between 50-70%, it’s a go-to for people who need effective relief without a lot of downtime.
That doesn't mean at-home care isn't important. It's absolutely crucial for managing symptoms and stopping small problems from turning into big ones. Even if you get a procedure done, things like maintaining a high-fiber diet and taking soothing sitz baths will help you heal and prevent new hemorrhoids from forming. The best strategy often involves using both approaches at different times on your journey to relief.
So, you’ve tried the suppositories, the sitz baths, and the lifestyle changes, but you’re still not getting enough relief. It’s a frustrating spot to be in, but it’s exactly when a doctor might bring up a minimally invasive procedure. These aren't major surgeries... they're effective, low-discomfort options performed right in the office that can offer lasting relief and get you back to your life quickly.
These procedures work by zeroing in on the internal hemorrhoid to either shrink it or cut off its blood supply. The three most common and trusted options are Infrared Coagulation (IRC), Sclerotherapy, and Rubber Band Ligation (RBL). Each has its own sweet spot, making them better suited for different types and grades of internal hemorrhoids. Knowing how they work can help you feel much more prepared when you talk with your doctor about what’s right for you.

Infrared Coagulation, or IRC, is a gentle and remarkably effective method for smaller, grade I and II internal hemorrhoids. It's a fantastic option if you're dealing with bleeding but don't have a significant prolapse (where the hemorrhoid bulges out). The procedure itself is quick, nearly painless, and requires no anesthesia.
During IRC, a small probe delivers a few short bursts of infrared light to the tissue just above the hemorrhoid. This light creates a tiny, controlled burn that triggers scar tissue to form. That scar tissue then cuts off the blood supply, causing the hemorrhoid to shrink and recede over the next week or two. Most people just describe it as a brief feeling of heat.
Since the 1980s, IRC has been a real game-changer. The non-surgical "zap" from its probe penetrates just 2.5 mm deep, but it boasts success rates of 67-96% when applied a few times per hemorrhoid. This makes it perfect for desk workers or adults over 50 who need a fast, low-pain office visit. Unlike surgery, there's minimal discomfort, no incisions, and you can usually get back to your day right after. You can discover more insights about these findings on the National Center for Biotechnology Information.
Sclerotherapy is another in-office procedure that works wonders for grade I and II internal hemorrhoids, especially those that mainly cause bleeding. Much like IRC, it’s fast, relatively painless, and doesn’t require sedation. The goal is simple: shrink the hemorrhoid by targeting its blood vessels directly.
Here’s the breakdown:
The injection itself usually isn't painful because it's given above the dentate line... an area inside the rectum with very few pain-sensing nerves. You might feel a bit of pressure or fullness, but that’s about it. Sclerotherapy is also a great choice for patients on blood thinners, since the risk of post-procedure bleeding is lower than with other options.
Sclerotherapy is often the go-to for patients with smaller internal hemorrhoids that are primarily causing bleeding. It's also a safe alternative for individuals where other procedures might carry a higher risk.
For more prominent or prolapsing internal hemorrhoids (grade II and III), Rubber Band Ligation (RBL) is often considered the most effective non-surgical treatment out there. It's been the reliable standard for decades, and for good reason... it has a high success rate and provides a long-term fix for many people.
During RBL, your doctor uses a special instrument to slip a tiny, tight rubber band around the base of the internal hemorrhoid. This simple move cuts off the blood supply completely. Without blood flow, the hemorrhoid starts to wither.
What to expect afterward:
While it’s highly effective, RBL isn't for everyone. It's typically reserved for hemorrhoids that are large enough to be banded and isn't used for external hemorrhoids. Your doctor will be able to tell if you’re a good candidate based on the size and grade of your internal hemorrhoids.
It can feel incredibly discouraging when at-home treatments and even standard in-office procedures fail to provide lasting relief. This is especially true for severe (grade 3-4) or stubborn internal hemorrhoids that just keep coming back.
For these challenging cases, advanced procedures offer powerful, long-term solutions that can finally break the cycle of pain and discomfort. They're typically reserved for when other methods have been exhausted, but they represent a more definitive step toward resolving the underlying issue.
One of the most effective advanced options is a specialized injection technique known as Polidocanol Sclerotherapy combined with ALTA (Aluminum Potassium Sulfate and Tannic Acid). This isn't your standard sclerotherapy. It’s a more potent formulation designed specifically for larger, more severe internal hemorrhoids that have prolapsed.
The procedure involves a precise injection into the hemorrhoidal tissue. This triggers an inflammatory reaction that hardens and shrinks the hemorrhoid over time, and it has shown remarkable results.
A significant 2006 comparative study found this technique had a 99% success rate at one year... even outperforming surgical hemorrhoidectomy, which had a 94% success rate. The study, involving over 3,500 patients, also showed that 98.1% reported positive effects within just 28 days. You can learn more about these powerful treatment findings and what they mean for severe cases.
This makes it an excellent choice for anyone needing a highly effective, non-surgical path to relief from grade 3 and 4 hemorrhoids.
Another modern technique gaining traction is Hemorrhoidal Artery Embolization (HAE). This minimally invasive, image-guided procedure is performed by an interventional radiologist, not a surgeon, and it takes a completely different approach by targeting the problem at its source: the blood flow.
The process is quite sophisticated:
By cutting off the blood supply, the hemorrhoids are starved of the oxygen and nutrients they need. As a result, they gradually shrink and decompress over the following weeks. This provides relief from symptoms like bleeding and prolapse without any cutting or tissue removal in the rectum itself.
Moving forward with an advanced procedure is a big decision, one you'll make in close consultation with a specialist like a colorectal surgeon or interventional radiologist. These treatments are typically recommended only after a thorough evaluation confirms that more conservative options aren’t working anymore.
Your doctor will consider several factors:
While these procedures are highly effective, they require specialized expertise and aren't as widely available as standard treatments like rubber band ligation. For those suffering from severe, recurring hemorrhoids, however, they represent the best internal hemorrhoid treatment available for achieving long-term freedom from symptoms.
Finding the right treatment for internal hemorrhoids isn't a one-size-fits-all deal. It becomes even more personal during sensitive times like pregnancy, postpartum recovery, or in our senior years. What works for one person might not be safe or effective for another, so it's crucial to adjust your approach based on specific health needs.

During these life stages, the goal shifts. You're not just looking for relief... you're looking for relief that’s both safe and gentle. The standard recommendations often need a second look to protect a mother and baby or to account for the unique health of older adults.
The immense pressure on the pelvic region during pregnancy and childbirth makes hemorrhoids a very common companion for new and expectant mothers. In fact, up to 40% of women deal with them during this time, but treatment choices have to be made with extra care.
The top concern is safety for both mom and baby. Many over-the-counter medications, especially those with steroids, are often off-limits. The focus shifts to gentle, OB/GYN-approved options that soothe without introducing any unnecessary risks.
Here are some of the safest and most effective strategies:
For new moms, consistency is everything. Combining gentle topicals with daily sitz baths and a high-fiber diet creates a healing environment that supports recovery. To learn more, check out our guide on how to treat hemorrhoids after childbirth.
For seniors, treating hemorrhoids is often about managing recurring flare-ups while being mindful of other health conditions. As we age, our tissues can weaken, and chronic issues like constipation might become more common, leading to persistent hemorrhoid problems.
Safety is still the top priority, but the focus broadens to include potential drug interactions and ease of use. Often, the most effective approach is a simple, reliable routine.
Key things for older adults to keep in mind:
Ultimately, whether for a new mom or a senior, the best internal hemorrhoid treatment is one chosen with care... prioritizing safety and addressing the unique needs of that life stage.
Most of the time, you can manage hemorrhoid flare-ups at home with sitz baths, dietary tweaks, or over-the-counter creams. But how do you know when it’s time to call in a professional? Certain symptoms are more than just a nuisance... they’re red flags that need a doctor's evaluation.
Ignoring persistent bleeding or truly unbearable pain isn't just toughing it out; it's risking complications like anemia or infection. Learning to spot these warning signs is the first step toward getting the right treatment.
Pay close attention to how your symptoms evolve. If things aren't getting better, or they suddenly get worse, it’s time to act. Don't brush these off.
Feeling a little anxious about a doctor's visit is normal, but being prepared can make the whole experience smoother and more productive.
Knowing how to react to specific symptoms ensures you get timely care.
| Symptom | Recommended Action |
|---|---|
| Fresh bleeding | Call your doctor within 48 hours. |
| Severe pain | Schedule an urgent consultation. |
| Irreducible prolapse | Seek a same-day evaluation. |
| Dizziness or weakness | Go to the emergency room immediately. |
This quick guide helps you match what you're feeling to the right course of action. It's about getting the proper care at the right moment.
Ignoring prolonged bleeding can lead to significant anemia and related health risks. It’s not something to take lightly.
For a closer look at what different types of bleeding might mean, check out our guide on bleeding hemorrhoids.
To get the most out of your appointment, a little prep work goes a long way.
Your doctor will likely perform a physical exam, which might include a digital rectal exam or an anoscopy to get a clear look at the internal tissue. Knowing this ahead of time can help ease any anxiety.
Once you have a clear diagnosis, your doctor will walk you through your options, which could range from stronger prescription medications to in-office procedures.
Follow their recommendations closely and don't be afraid to reach out if new questions or concerns pop up. Taking that first step to see a professional is often the hardest part, but it puts you on the direct path to lasting relief.
Got questions about finding relief? You're not alone. Here are some straightforward answers to help you navigate your treatment options with confidence.
Most people start to feel some initial relief from itching and discomfort within the first day. Once a suppository is inserted, it dissolves and delivers active ingredients like phenylephrine directly to the swollen tissue, getting to work fast.
But for the full shrinking effect, you need to be consistent. Using them as directed for several days gives the medication enough time to calm the inflammation and let the hemorrhoid heal properly.
Yes, and it’s usually a great first step. Many doctors actually recommend starting with conservative, at-home treatments before considering anything more invasive.
A quality suppository can often manage the symptoms so well that the flare-up resolves on its own, meaning you might not even need a procedure. If you do end up needing one, using soothing products beforehand can help reduce inflammation, which might make the treatment itself more comfortable. Just be sure to tell your doctor what OTC products you're using.
For the fastest relief at home, you’ll want to tackle the problem from a few different angles at once. A combination approach is almost always the most effective strategy.
Try this simple but powerful routine:
This three-part plan addresses the internal cause, soothes the surrounding area, and protects sensitive skin all at once. It’s one of the best strategies you can follow at home for comprehensive, fast-acting results.
For a safe, steroid-free approach to managing internal hemorrhoids, trust the targeted relief of Revivol-XR Hemorrhoid Suppositories. They’re designed to shrink swollen tissue and soothe irritation, helping you get back to feeling like yourself. Explore our full range of doctor-trusted solutions at hemorrhoid.com.